Women Infertility: A Systematic Review of Effects and Causes

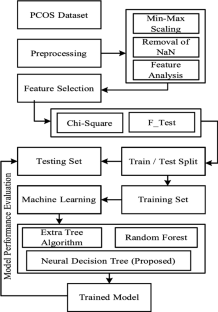
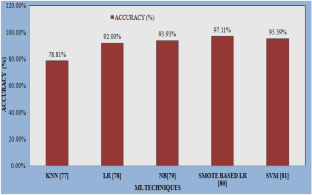
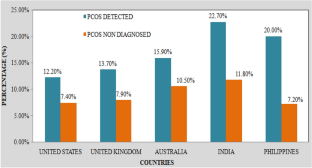
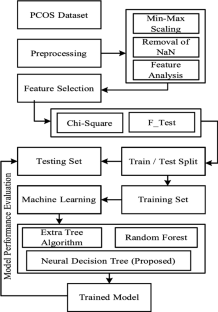
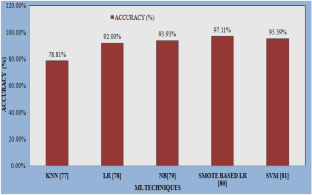
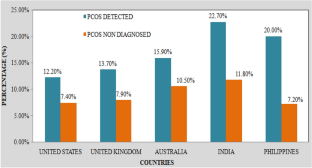
Recently, infertility has been affecting a large number of women than men. It is the male or female reproductive system’s disease. Consequently, after 12 months or more of usual insecure sexual intercourse, if they fail to attain pregnancy then that failure is defined as infertility. As per the National Institute of Child Health and Human Development, people in the USA have infertility issues that are found in 11% of women along with 9% of men. Women are more fertile in their 20s, while in their 30s it reduces to half of it. After 35 years, the probability of getting pregnant is diminished in women. For the woman to get pregnant, the proper functioning of the ovaries, fallopian tubes, and uterus is required. So, infertility occurs due to any issues with the above body parts. Women's infertility is caused by many factors, but the most vital cause is polycystic ovary syndrome (PCOS), which is a hormonal disorder commonly found among reproductive-aged women. So, women infertility, effects of women infertility, causes of women infertility, PCOS and detection of PCOS by general and machine learning (ML) techniques had been discussed in this paper. The accuracy attained in the detection of PCOS utilizing ML techniques is analyzed. Among people as of the top five responding countries that incorporate the USA, UK, Australia, India, together with the Philippines, the percentage of women with physician-assured PCOS against women exclusive of PCOS is analyzed.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save
Springer+ Basic
€32.70 /Month
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Buy Now
Price includes VAT (France)
Instant access to the full article PDF.
Rent this article via DeepDyve
Similar content being viewed by others

Polycystic Ovary Syndrome (PCOS) diagnostic methods in machine learning: a systematic literature review
Article 27 June 2024

Chapter © 2023

Prediction of Polycystic Ovary Syndrome (PCOS) Using Optimized Machine Learning Classifiers
Chapter © 2023
Explore related subjects
References
- Melodie Vander B, Christineyns W. Fertility and infertility definition and epidemiology. Clin Biochem. 2018;62:2–10. Google Scholar
- American Society for Reproductive Medicine. Infertility an overview a guide for patients. 2017. https://www.reproductivefacts.org/globalassets/rf/news-and-publications/bookletsfact-sheets/english-fact-sheets-and-info-booklets/infertility-an_overview_booklet2.pdf.
- Mara M, Laura C, Manuela U, Emanuele P. Editorial female infertility genetics of reproductive ageing, menopause and primary ovarian insufficiency. Front Genet. 2022;13:1–3. Google Scholar
- Narjes D, Tina M, Meimanat H. Infertility related risk factors a systematic review. Int J Women’s Health Reprod Sci. 2017;5(1):24–9. Google Scholar
- Shahnaz A, Ayesha A. Infertility a review on causes, treatment and management. Women’s Health Gynecol. 2016;2(6):1–5. Google Scholar
- Murtaza M, Sharifa AM, Janan H, Iiizam EM, Aliya S. Male and female infertility causes, and management. IOSR J Dent Med Sci. 2019;18(9):27–32. Google Scholar
- Female Infertility. Cleveland Clinic, 2020, https://my.clevelandclinic.org/health/diseases/17774-female-infertility.
- ZeynepOzcan D, Berna D. Impact of obesity on infertility in women. J Turk German Gynecol Assoc. 2015;16(2):111–7. Google Scholar
- Female infertility. Mayo Clinic, 2021, https://www.mayoclinic.org/diseases-conditions/female-infertility/symptoms-causes/syc-20354308.
- M. Ashraf Direkvand, D. Ali and A. Khosravi. Epidemiology of female infertility a review of literature. Biosciences.
- Barbieri RL. Female infertility. 8th ed. Elsevier; 2019. (ISBN: 978-0-323-47912-7). Google Scholar
- Nardo LG, Chouliaras S. Definitions and epidemiology of unexplained female infertility. Obstet Gynecol Surv. 2015;69(2):109–15. Google Scholar
- Ogawa M, Takamatsu K, Horiguchi F. Evaluation of factors associated with the anxiety and depression of female infertility patients. BioPsychoSocial Med. 2011;5:1–5. Google Scholar
- Simi MS, Sankara Nayaki K, Parameswaran M, Sivadasan S. Exploring female infertility using predictive analytic. In: Global Humanitarian Technology Conference, IEEE, 9–22 October 2017, San Jose, CA, USA 2017.
- Brazdova A, Senechal H, Peltre G, Poncet P. Immune aspects of female infertility. Int J Fertil Steril. 2016;10(1):1–10. Google Scholar
- Mori K, Kitaya K, Ishikawa T, Hata Y. Analysis of endometrium form by using l bp for female infertility. In: International Conference on Machine Learning and Cybernetics, 15–18 July 2018, Chengdu, China, 2018.
- Nishihara R, Matsubayashi H, Ishikawa T, Hata H. Automated diagnosis of the frequency of uterine peristalsis for female infertility. In: 50th International Symposium on Multiple-Valued Logic, IEEE, 09–11 November 2020, Miyazaki, Japan, 2020.
- Kabadi YM, Harsha B. Hysterolaparoscopy in the evaluation and management of female infertility. J Obstet Gynecol India. 2016;66:478–81. Google Scholar
- Moghadam AD, Delpisheh A, Direkvand-Moghadam A. Effect of infertility on sexual function a cross-sectional study. J Clin Diagn Res. 2015;9(5):1–3. Google Scholar
- Salomao PB, Navarro PA, Romao APMS, Lerri MR, da Silva Lara LA. Sexual function of women with infertility. Revista Brasileira de Ginecologiae Obstetrícia. 2018;40(12):771–8. Google Scholar
- Webair HH, Ismail TAT, Ismail SB, et al. Patient-centered infertility questionnaire for female clients (PCIQ-F) part I questionnaire development. BMC Med Res Methodol. 2021;21(1):1–10. Google Scholar
- Kashi AM, Moradi Y, Chaichian S, Najmi Z, Mansori K, Salehin F, Rastgar A, Khateri S. Application of the World Health Organization Quality of Life Instrument, Short Form (WHOQOL-BREF) to patients with endometriosis. Obstet Gynecol Sci. 2018;61(5):598–604. Google Scholar
- Aimagambetova G, Issanov A, Terzic S, Bapayeva G, Ukybassova T, Baikoshkarova S, Aldiyarova A, Shauyen F, Terzic M. The effect of psychological distress on IVF outcomes reality or speculations. PLoS ONE. 2020;15(12):1–14. Google Scholar
- Wdowiak A, Anusiewicz A, Bakalczuk G, Raczkiewicz D, Janczyk P, Makara-Studzinska M. Assessment of quality of life in infertility treated women in Poland. Int J Environ Res Public Health. 2021;18(8):1–13. Google Scholar
- Maroufizadeh S, Riazi H, Lotfollahi H, Omani-Samani R, Amini P. The 6-item Female Sexual Function Index (FSFI-6) factor structure, reliability, and demographic correlates among infertile women in Iran. Middle East Fertil Soc J. 2019;24:1–6. Google Scholar
- Al-Homaidan HT. Depression among women with primary infertility attending an infertility clinic in Riyadh, Kingdom of Saudi Arabia rate, severity, and contributing factors. Int J Health Sci Qassim Univ. 2011;5(2):108–15. Google Scholar
- Bakhtiyar K, Beiranvand R, Ardalan A, Changaee F, Almasian M, Badrizadeh A, Bastami F, Ebrahimzadeh F. An investigation of the effects of infertility on women’s quality of life a case–control study. BMC Womens Health. 2019;19:1–9. Google Scholar
- What are some possible causes of female infertility. 2017, https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/causes/causes-female
- Amudha M, Rani S, Kannan K, Manavalan R. An updated overview on causes, diagnosis and management of infertility. Int J Pharm Sci Rev Res. 2013;18(1):155–64. Google Scholar
- Hernandez-Angeles C, Castelo-Branco C. Early menopause a hazard to a woman’s health. Indian J Med Res. 2016;143(4):420–7. Google Scholar
- Mafra FA, Christofolini DM, Cavalcanti V, Vilarino FL, Andre GM, Kato P, Bianco B, Barbosa CP. Aberrant telomerase expression in the endometrium of infertile women with deep endometriosis. Arch Med Res. 2014;45:31–5. Google Scholar
- Carranza-Mamane B, Havelock J, Hemmings R. The management of uterine fibroids in women with otherwise unexplained infertility. Pract Guidel. 2015;37(3):277–85. Google Scholar
- Cook AS, David-Adamson G. The role of the endometriosis fertility index (EFI) and endometriosis scoring systems in predicting infertility outcomes. Curr Obstet Gynecol Rep. 2013;2(3):186–94. Google Scholar
- Koninckx PR, Ussia A, Keckstein J, Adamyan L, Wattiez A, Martin DC. Prevalence of endometriosis and peritoneal pockets in women with infertility and/or pelvic pain. Gynaecol Gynaecol. 2021;43(8):935–42. Google Scholar
- Santoso B, Rahmawati NY, Saadi A, Dwiningsih SR, Annas JY, Tunjungseto A, Ardianta-Widyanugraha MY, Mufid AF, Ahsan F. Elevated peritoneal soluble endoglin and GDF-15 in infertile women with severe endometriosis and pelvic adhesion. J Reprod Immunol. 2021;146:1–10. Google Scholar
- Yasui T, Hayashi K, Mizunuma H, Kubota T, Asod T, Matsumura Y, Lee JS, Suzuki S. Association of endometriosis-related infertility with age at menopause. Maturitas. 2011;69:279–83. Google Scholar
- Huang H, Kuang H, Sun F, et al. Lower prevalence of non-cavity distorting uterine fibroids in patients with polycystic ovary syndrome than in those with unexplained infertility. Fertil Steril. 2019;111(5):1011–9. Google Scholar
- Huang S, Du X, Wang R, Li R, Wang H, Luo L, O’Leary S, Qiao J, Mol BWJ. Ovulation induction and intrauterine insemination in infertile women with polycystic ovary syndrome a comparison of drugs. EURO. 2018;231:117–21. Google Scholar
- Vannuccini S, Clifton VL, Fraser IS, Taylor HS, Critchley H, Giudice LC, Petraglia F. Infertility and reproductive disorders impact of hormonal and inflammatory mechanisms on pregnancy out-come. Hum Reprod Update. 2016;22(1):104–15. Google Scholar
- Yang X-J. Telocytes in inflammatory gynaecologic diseases and infertility. Adv Exp Med Biol. 2016;913:263–85. Google Scholar
- Dennett CC, Simon J. The role of polycystic ovary syndrome in reproductive and metabolic health over- view and approaches for treatment. Diabetes Spectr. 2015;28(2):116–20. Google Scholar
- Mondal S. Polycystic ovary syndrome. Lecture Notes, 2020, https://doi.org/10.13140/RG.2.2.22872.03840.
- Mahoney D. Lifestyle modification intervention among infertile overweight and obese women with polycystic ovary syndrome. J Am Assoc Nurse Pract. 2014;26:301–8. Google Scholar
- Kumar AN, Naidu JN, Satyanarayana U, Ramalingam K, Anitha M. Metabolic and endocrine characteristics of Indian women with polycystic ovary syndrome. Int J Fertil Steril. 2016;10(1):22–8. Google Scholar
- Wright PJ, Dawson RM, Corbett CF. Social construction of biopsychosocial and medical experiences of women with polycystic ovary syndrome. J Adv Nurs. 2020;76:1728–36. Google Scholar
- Neagu M, Cristescu C. Anti-Mullerian hormone a prognostic marker for metformin therapy efficiency in the treatment of women with infertility and polycystic ovary syndrome. J Med Life. 2012;5(4):462–4. Google Scholar
- Tayrab E, Ali M, Modawe GA, Naway L, Abdrabo AEA. Serum Anti-Müllerian hormone as laboratory predictor in infertile women with and without polycystic ovary syndrome. Am J Res Commun. 2014;2(3):61–6. Google Scholar
- Wang C, Wei Wu, Yang H, Ye Z, Zhao Y, Liu J, Liangshan Mu. Mendelian randomization analyses for PCOS: evidence, opportunities and challenges. Trends Genet. 2022;38(5):468–82. Google Scholar
- Fetouh AA, Mohamed RS. Ovarian Doppler study in polycystic ovary syndrome in relation to body weight. Al-AzharAssiut Med J. 2015;13(3):34–42. Google Scholar
- Lujan ME, Jarrett BY, Brooks ED, Reines JK, Peppin AK, Muhn N, Haider E, Pierson RA, Chizen DR. Updated ultrasound criteria for polycystic ovary syndrome reliable thresholds for elevated follicle population and ovarian volume. Hum Reprod. 2013;28(5):1361–8. Google Scholar
- Lee TT, Rausch ME. Polycystic Ovarian Syndrome: role of imaging in diagnosis. Radio Graph. 2012;32(6):1643–57. Google Scholar
- Rachana B, Priyanka T, Sahana KN, Supritha TR, Parameshachari DB, Sunitha R. Detection of polycystic ovarian syndrome using follicle recognition technique. Glob Trans Proc. 2021;2(2):304–8. Google Scholar
- Ali HI, Elsadawy ME, Khater NH. Ultrasound assessment of polycystic ovaries Ovarian volume and morphology; which is more accurate in making the diagnosis. Egypt J Radiol Nucl Med. 2016;47:347–50. Google Scholar
- Tsymbal S. 5 essential machine learning algorithms for business applications. 2020, https://mobidev.biz/blog/5-essential- machine-learning-techniques.
- Garg S, Wadi MKS, Garg B. Color Doppler as diagnostic criteria in polycystic ovarian syndrome. Int J Clin Obstet Gynaecol. 2021;5(2):8–11. Google Scholar
- Mehr HD, Polat H. Diagnosis of poly- cystic ovary syndrome through different machine learning and feature selection techniques. Health Technol. 2021;12(1):137–50. Google Scholar
- Hassan MM, Mirza T. Comparative analysis of machine learning algorithms in diagnosis of polycystic ovarian syndrome. Int J Comput Appl. 2020;175(17):42–53. Google Scholar
- Renju K, Pavithra B. Comparative analysis of classifiers for predicting polycystic ovary syndrome using deep learning models. J Emerg Technol Innov Res. 2022;9(6):291–7. Google Scholar
- Thakre V, Vedpathak S, Thakre K, Sonawani S. PCOcare PCOS detection and prediction using machine learning algorithms. Biosci Biotechnol Res Commun. 2020;13(14):240–4. Google Scholar
- Vikas B, Anuhya BS, Chilla M, Sarangi S. A critical study of polycystic ovarian syndrome (PCOS) classification techniques. Int J Comput Eng Manag. 2018;21(4):1–7. Google Scholar
- Purnama B, Wisesti UN, Adiwijaya, Nhita F, Gayatri A, Mutiah T. A classification of polycystic ovary syndrome based on follicle detection of ultra- sound images. In: 3rd International Conference on Information and Communication Technology, 27–29 May 2015, Nusa Dua, Bali, Indonesia, 2015.
- Tanwani N. Detecting PCOS using machine learning. Int J Modern Trends Eng Sci. 2020;7(1):1–7. Google Scholar
- Mehrotra P, Chatterjee J, Chakraborty C, Ghoshdastidar B, Ghoshdastidar S. Automated screening of polycystic ovary syndrome using machine learning techniques. In: Annual IEEE India Conference, 16–18 December 2011, Hyderabad, India, 2011.
- Dutta P, Paul S, Majumder M. An efficient smote based machine learning classification for prediction & detection of PCOS. 2021, https://doi.org/10.21203/rs.3.rs-1043852/v1.
- Nilofer NS, Ramkumar R. Follicles classification to detect polycystic ovary syndrome using GLCM and novel hybrid machine learning. Turk J Comput Math Educ. 2021;12(7):1062–73. Google Scholar
- Denny A, Raj A, Ashok A, Maneesh Ram C, George R. i-HOPE detection and prediction system for polycystic ovary syndrome (PCOS) using machine learning techniques. In: TENCON 2019—2019 IEEE Region 10 Conference, 17–20 October 2019 Kochi, India, 2019.
- Jain T, Negris O, Brown D, Galic I, Salimgaraev R, Zhaunova L. Characterization of polycystic ovary syndrome among Floapp users around the world. Reprod Biol Endocrinol. 2021;19:1–11. Google Scholar
Funding
No funding was received for this research work.